✔ 100% Authentic Product
👁️ Currently Viewing 1782
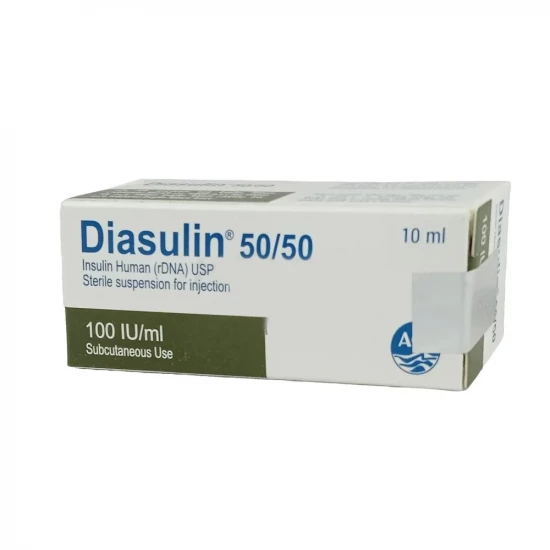
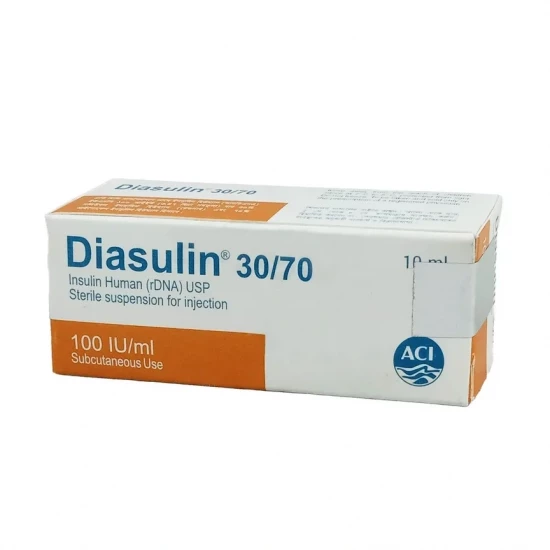
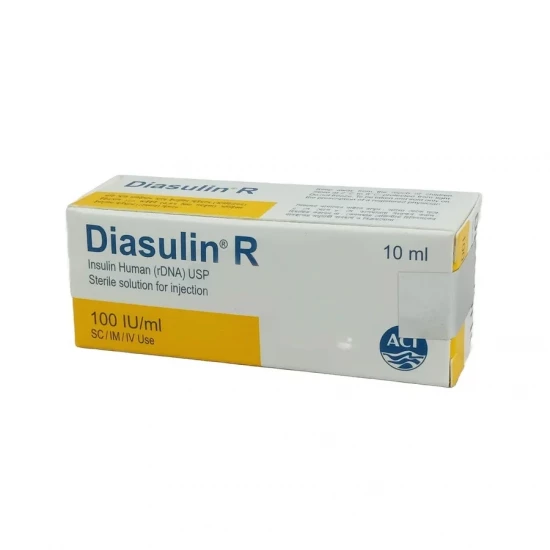
Diasulin R Vial 100 IU/ml
Diasulin R 100 IU/ml Injection (Human Insulin rDNA)
Diabetes Mellitus (Type 1 and Type 2)
Diabetic Ketoacidosis (DKA)
Hyperkalemia (as adjunct therapy with glucose infusion)
Discount
Price: ৳ 407
MRP:
৳
415
2%
Off

100% Genuine Products, Guaranteed

Safe & Secure Payments, Always
Fast, Secure & Efficient Delivery
Proper Packaging
 Cash on Delivery - All over Bangladesh
Cash on Delivery - All over Bangladesh Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59
Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59 Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110
Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110
 ফ্রি ডেলিভারিঃ - ৯৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে
ফ্রি ডেলিভারিঃ - ৯৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে ফ্রি ডেলিভারিঃ - ২৯৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
ফ্রি ডেলিভারিঃ - ২৯৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
100% Genuine Products, Guaranteed
Safe & Secure Payments, Always
Fast, Secure & Efficient Delivery
Proper Packaging
 Cash on Delivery - All over Bangladesh
Cash on Delivery - All over Bangladesh Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59
Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59 Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110
Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110 ফ্রি ডেলিভারিঃ - ৯৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে
ফ্রি ডেলিভারিঃ - ৯৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে ফ্রি ডেলিভারিঃ - ২৯৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
ফ্রি ডেলিভারিঃ - ২৯৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
✅ Description:
Diasulin R (Regular Human Insulin) is a short-acting insulin that regulates carbohydrate, protein, and fat metabolism.
It reduces blood glucose by:
- Promoting glucose uptake in muscle and adipose tissues
- Suppressing hepatic glucose production
- Inhibiting lipolysis and proteolysis
It has a rapid onset (30 minutes), peak effect at 1–3 hours, and duration of 6–8 hours.
Intravenous administration produces immediate glucose-lowering effects, while subcutaneous absorption is slower.
✔️ Dosage & Administration
Adult Dosage
Type 1 Diabetes Mellitus:
Initial: 0.2–0.4 units/kg/day SC divided every 8 hours or more frequently
Maintenance: 0.5–1 unit/kg/day (higher doses may be required in insulin-resistant patients)
Type 2 Diabetes Mellitus:
Initial: 0.2–0.4 units/kg/day SC divided every 8–12 hours, as adjunct to diet, exercise, or oral agents
Diabetic Ketoacidosis (IV route):
Initial loading dose: 20 units
Continuous infusion: 6 units/hour until blood glucose falls to ~10 mmol/L
Adjust: Reduce to 3 units/hour with 5% glucose infusion to avoid hypoglycemia
Continue until patient resumes oral intake
Hyperkalemia:
5–10 units IV insulin in 50 mL D50W (25 g glucose) infused over 15–30 minutes
Combination with Intermediate-acting Insulin:
Morning: ⅔ of daily insulin dose (Regular:NPH = 1:2)
Evening: ⅓ of daily insulin dose (Regular:NPH = 1:1)
Pediatric Dosage
Type 1 Diabetes Mellitus:
Initial: 0.2–0.4 units/kg/day SC
Maintenance: 0.5–1 unit/kg/day; may increase up to 1.5 units/kg/day during puberty
Prepubertal children: Usually require 0.7–1 unit/kg/day
Special Populations
Renal impairment: Dose reduction may be necessary
Hepatic impairment: Use with caution; dosage adjustment required
✔️ Administration Route
Subcutaneous (preferred): Inject into the upper arm, thigh, or abdominal wall.
Intravenous (IV): For DKA management under close monitoring.
Intramuscular (IM): In emergencies when IV access is not available.
Administer within 15 minutes before or immediately after meals.
Abdominal injections ensure faster absorption.
✔️ Side Effects
Common: Hypoglycemia, headache, blurred vision, rash, pruritus
Local: Injection site reactions, lipodystrophy, lipoatrophy
Systemic: Allergic reactions, insulin resistance, hypokalemia, flu-like symptoms, back pain, diarrhea, dyspepsia, pharyngitis
✔️ Drug Interactions
↓ Hypoglycemic effect (antagonistic):
Corticosteroids, diuretics, thyroid hormones, danazol, glucagon, sympathomimetics, oral contraceptives, atypical antipsychotics
↑ Hypoglycemic effect (synergistic):
Oral antidiabetic agents, ACE inhibitors, MAOIs, salicylates, fibrates, fluoxetine, sulfonamide antibiotics
Others:
Beta-blockers may mask hypoglycemia symptoms
Alcohol can potentiate or prolong hypoglycemia
Pioglitazone/Rosiglitazone may increase weight gain and edema risk
✔️ Contraindications
Hypoglycemia
Hypersensitivity to human insulin or formulation components
✔️ Precautions
Monitor blood glucose regularly and adjust dose accordingly
Pregnancy: Insulin needs may vary — lower in the 1st trimester, higher in 2nd & 3rd
Lactation: Safe to use; dosage adjustment may be required
Caution in conditions with decreased insulin requirement (renal/hepatic impairment, malabsorption, hypothyroidism)
Caution in conditions with increased insulin requirement (fever, infection, surgery, trauma)
Hypokalemia may occur; monitor potassium levels
✔️ Storage
Store at 2°C–8°C (refrigerated). Do not freeze.
Protect from light.
In-use vials can be kept below 25°C for up to 6 weeks.
⚠️Disclaimer:
At ePharma, we’re committed to providing accurate and accessible health information. However, all content is intended for informational purposes only and should not replace medical advice from a qualified physician. Please consult your healthcare provider for personalized guidance. We aim to support, not substitute, the doctor-patient relationship.